Table of Contents
How blood sugar test is done A blood sugar metre is required for blood sugar testing. The metre detects the quantity of sugar in a tiny sample of blood, commonly taken from your fingertip and placed on a disposable test strip. Even if you use a CGM, you’ll need a blood sugar metre to calibrate it on a regular basis.
A suitable gadget might be recommended by your health care practitioner or trained diabetes care and education professional. He or she may also instruct you on how to utilise your metre.
Follow the instructions included with your blood sugar metre. In general, the procedure is as follows:
Wash and dry your hands thoroughly. (Food and other things may cause an incorrect reading.)
- Place a test strip in your metre.
- Prick your fingers on the side with the needle (lancet) that came with your test kit.
- Touch and hold the test strip’s edge to the drop of blood.
- After a few seconds, the metre will reveal your blood sugar level on a screen.
Some metres may test blood from a different location, such as the forearm or palm. However, these measurements may not be as reliable as readings taken from the fingers, particularly after a meal or after activity, when blood sugar levels fluctuate more often. Alternative locations are not advised for CGM calibration.
1 Why test your blood sugar
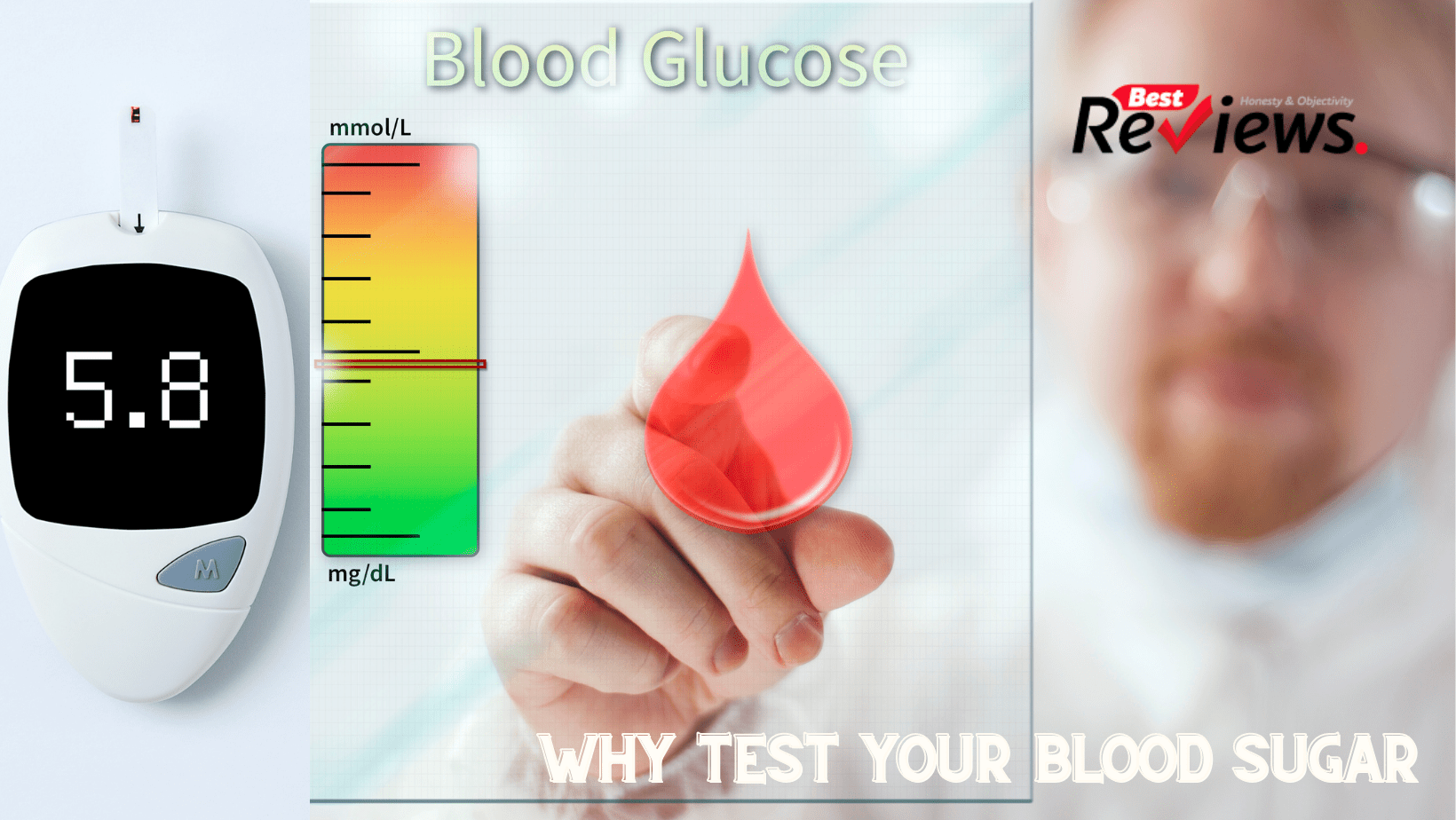
Blood sugar measurement gives valuable data for diabetes management. It can assist you with:
- Keep track of how diabetes treatments affect blood sugar levels.
- Determine if your blood sugar levels are high or low.
- Keep track of your progress toward your overall treatment objectives.
- Discover how nutrition and exercise influence blood sugar levels.
- Recognize how other variables, such as sickness or stress, influence blood sugar levels.
2 When to test your blood sugar
Your doctor will tell you how often you should monitor your blood sugar levels. The frequency of testing is typically determined by the type of diabetes and the treatment strategy.
3 Type 1 diabetes
If you have type 1 diabetes, your doctor may advise you to test your blood sugar 4 to 10 times a day. You may need to run the following tests:
- Prior to meals and snacks
- Exercise before and after
- Before going to bed
- Throughout the night (sometimes)
- If you’re sick, this happens more often.
- More often if you alter your usual routine
- More often if you begin a new medicine
4 Type 2 diabetes
If you use insulin to control type 2 diabetes, your doctor may advise you to test your blood sugar multiple times each day, depending on the kind and quantity of insulin you use. If you take many daily injections, testing is typically indicated before meals and after night. If you only take intermediate- or long-acting insulin, you may only need to test before breakfast and possibly before supper or at sleep.
You may not need to test your blood sugar on a regular basis if you manage type 2 diabetes with noninsulin drugs or diet and exercise alone.
5 What if you have a continuous glucose monitor (CGM)?
CGMs may also be used by people with diabetes, especially those with type 1 diabetes. These gadgets use a sensor implanted under the skin to test your blood sugar every few minutes. These sensors are usually used for a week or two before needing to be replaced.
The most recent continuous glucose monitor has an implanted sensor that can track blood sugar levels for up to three months. A transmitter worn on the body wirelessly transmits blood sugar readings from the sensor to a smartphone app.
Some systems display your blood sugar level on a receiver, smartphone, or wristwatch at all times, and an alert sounds if your blood sugar rises or falls too rapidly. Others need you to monitor your blood sugar by frequently running the receiver over the sensor.
To calibrate the equipment, most of these devices still need finger-stick examinations. Check the user manual for your gadget to see whether you need to check it and, if so, how often.
Certain drugs, including acetaminophen (Tylenol and others), albuterol (Proair HFA, Ventolin HFA, and others), and lisinopril (Prinivil, Zestril, and Qbrelis), may impair the accuracy of certain CGM readings, especially on earlier types of CGMs. Standard acetaminophen dosages seem to have no effect on readings on newer CGMs (up to 1,000 milligrammes for an adult).
If you must take drugs that may impair the accuracy of the readings, your doctor may advise you to double-check your CGM findings with a regular blood sugar metre. If you are pregnant, on dialysis, or seriously sick, see your health care practitioner before wearing a CGM, since these situations may impact the blood sugar readings from a CGM.
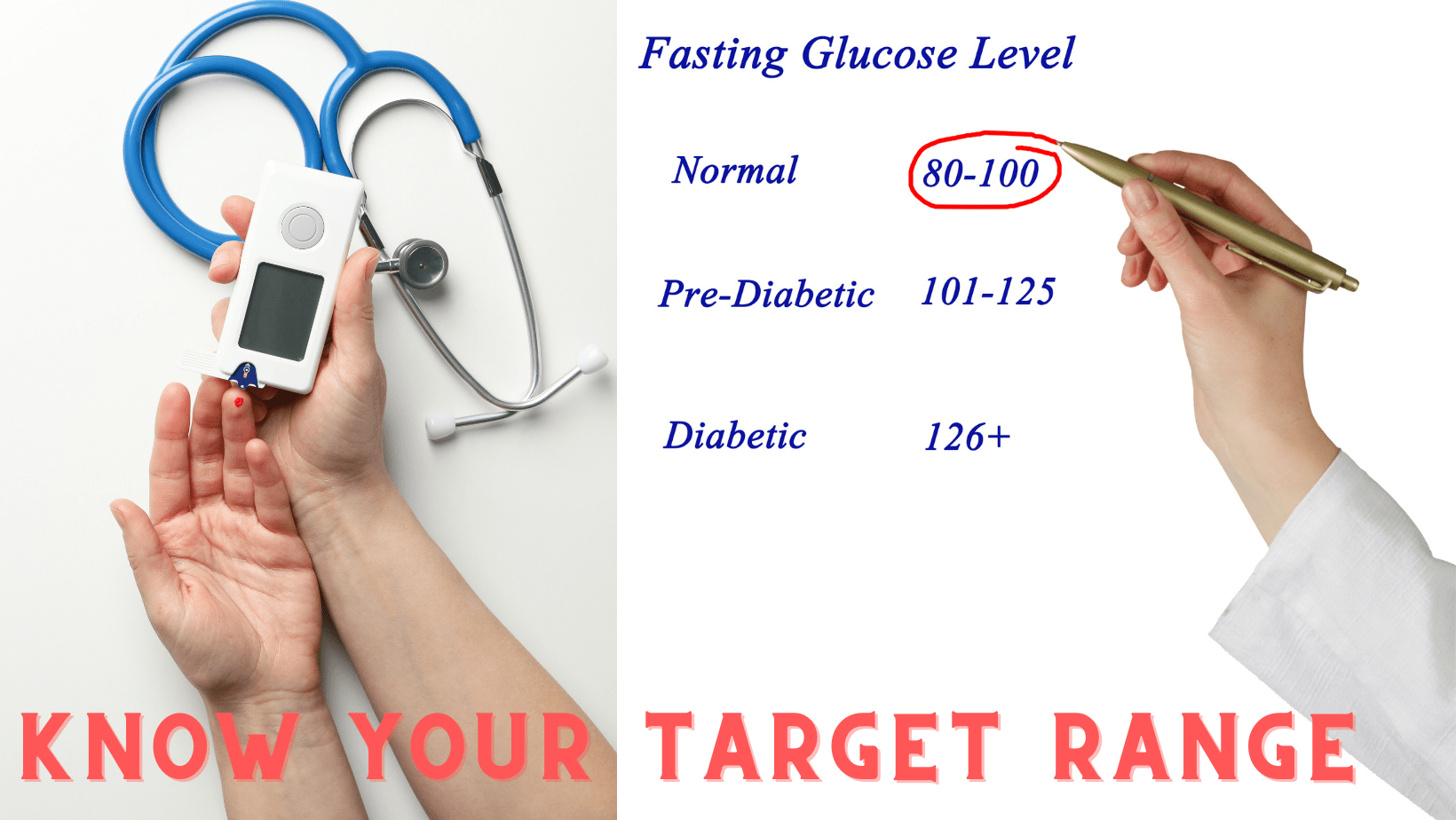
6 Know your target range
Inquire with your doctor about a safe blood sugar level for you. Your doctor will determine target blood sugar test results depending on various criteria, including:
- Diabetes kind and severity
- Age
- How long have you had diabetes?
- Status of pregnancy
- Diabetes problems are present.
- The general state of health and the existence of various medical disorders
The American Diabetes Association (ADA) recommends the following blood sugar values as a general guideline:
- Before meals, take 80 to 130 milligrammes per deciliter (mg/dL) or 4.4 to 7.2 millimoles per litre (mmol/L).
- Two hours after meals, less than 180 mg/dL (10.0 mmol/L).
However, the ADA emphasises that these objectives frequently change based on your age and personal health and should be tailored to your specific needs.
Some persons will have somewhat higher blood sugar targets, such as those who:
- are above the age of 60
- Have any other medical issues, such as heart disease, lung disease, or renal disease?
- Have a diminished capacity to detect low blood sugar levels (hypoglycemia unawareness)

















